Healthcare App Development: The 7-Step Simplified Guide [2026]
Healthcare organizations are under increasing pressure to deliver better patient experiences, improve clinical efficiency, and meet strict data-privacy regulations—while operating with limited resources and complex legacy systems. As a result, healthcare app development is no longer a “nice-to-have”, but a strategic investment for hospitals, clinics, insurers, and digital health startups worldwide.
However, building a healthcare app is fundamentally different from developing apps in other industries. Many organizations struggle not because of technology, but because they start without a clear scope, underestimate compliance requirements, or over-engineer solutions before validating real-world impact.
This healthcare app development guide breaks the process into seven practical, risk-reduced steps—from defining user groups and compliance scope to MVP development, testing, deployment, and continuous improvement. The focus is on clarity, measurability, and faster time to value, helping decision-makers evaluate use cases, costs, compliance, and whether building an app is the right move.
Table of Contents
- What Is Healthcare App Development?
- Types of Healthcare Apps
- 10 Benefits for Healthcare Providers and Patients
- Must-Have Features for a Modern Healthcare App
- Most Common Healthcare App Use Cases
- The 7-Step Simplified Healthcare App Development Process
- Costs of Healthcare App Development in 2026
- Strategic Analysis: Challenges, Decisions, and Investment Readiness
- How to Choose the Right Healthcare App Development Partner
- Why Choose Kaopiz for Healthcare App Development in Singapore
- Emerging Trends Transforming Healthcare Apps in 2026
- Conclusion
- FAQs
What Is Healthcare App Development?
Healthcare app development is the process of designing, building, and maintaining digital applications that support healthcare delivery, patient engagement, clinical workflows, and medical data management—while complying with strict regulations such as PDPA, HIPAA, and GDPR.
The global healthcare mobile application market was valued at $114.17 billion in 2024 and is projected to reach $1,070.58 billion by 2030, growing at a CAGR of 45.2% between 2025 and 2030. This explosive growth reflects a global shift toward digital health solutions, driven by rising smartphone penetration, increased chronic disease prevalence, and growing demand for accessible healthcare.

Unlike standard mobile or web apps, healthcare applications must operate within highly regulated environments. They handle sensitive health data, integrate with clinical systems (such as EHR/EMR, lab systems, or insurance platforms), and support multiple user groups—including patients, healthcare providers, administrators, and third-party partners. As a result, security, interoperability, accessibility, and reliability are as critical as user experience.
Types of Healthcare Apps
App development for healthcare can be grouped into three core categories based on who uses them and what problems they solve. Understanding these categories helps organizations define scope correctly, avoid unnecessary features, and prioritize ROI from the start.
Patient-Facing Apps
Patient-facing healthcare apps are designed to improve access, engagement, and continuity of care. They focus on empowering patients to interact with healthcare services more conveniently and proactively.
Common examples include:
- Appointment booking and reminders
- Telemedicine and virtual consultations
- Personal health records and test result access
- Medication reminders and adherence tracking
- Remote patient monitoring via wearable or IoT devices
- AI-powered symptom checkers and health assistants
Key considerations for patient-facing apps include usability, accessibility, and trust. In healthcare, many users are elderly or non-technical, so features such as large fonts, simple navigation, multilingual support, and clear consent flows are critical. Strong data privacy controls are also essential, as patients directly interact with sensitive medical information.
Provider-Facing Apps
Provider-facing apps support doctors, nurses, clinicians, and care teams in delivering care more efficiently and accurately. These applications are often workflow-centric and deeply integrated with existing clinical systems.

Typical use cases include:
- Clinical documentation and electronic health record (EHR/EMR) access
- Care coordination and task management
- Clinical decision support and alerts
- Prescription management and order entry
- Secure internal communication between care teams
Unlike patient apps, provider-facing tools must prioritize speed, reliability, and integration over visual complexity. Poor performance or workflow friction can directly impact care quality, making system stability, offline support, and role-based access control especially important.
Operational & Workflow Optimization Apps
Operational healthcare apps focus on administrative efficiency, cost control, and system-level optimization. While less visible to patients, these applications are often critical for scalability and long-term sustainability.
Common examples include:
- Staff scheduling and workforce management
- Billing, claims processing, and insurance integration
- Reporting, analytics, and regulatory compliance tracking
- Inventory and asset management
- System integration platforms connecting EHRs, labs, pharmacies, and insurers
These apps are typically built as web platforms or internal systems and must handle complex rules, high data volumes, and multiple integrations. Security, auditability, and interoperability are key requirements, especially for large hospital groups and insurance providers.
10 Benefits for Healthcare Providers and Patients
Healthcare app development delivers value on both sides of the care journey—improving operational efficiency for providers while enhancing accessibility, engagement, and outcomes for patients. Below are the key benefits healthcare organizations and patients gain when digital health solutions are designed and implemented correctly.
Benefits for Healthcare Providers
Well-designed healthcare apps create measurable value for providers by improving efficiency, care quality, and long-term sustainability. Below are five key benefits, supported by industry data.

1. Improved Operational Efficiency & Reduced Administrative Burden
Healthcare apps automate scheduling, documentation, and reporting, significantly reducing manual workloads. Clinicians can spend 30–40% of their time on administrative tasks, while digital workflow tools can reduce this burden by 20–30%, freeing more time for patient care.
2. Better Clinical Decision-Making with Data & AI
Provider-facing apps unify data from EHRs, labs, and devices into a single view. When combined with AI-driven insights, clinicians can make faster, more accurate decisions. McKinsey reports that data-driven healthcare organizations can improve clinical outcomes by 15–20%.
3. Lower Costs and Smarter Resource Utilization
Healthcare apps help reduce no-shows, optimize staffing, and avoid duplicate tests. Telehealth and remote monitoring alone can cut unnecessary in-person visits by 20–40%, lowering costs without impacting care quality.
4. Stronger Compliance, Security, and Audit Readiness
Modern healthcare apps support PDPA, HIPAA, and GDPR through built-in security features such as role-based access, audit logs, encryption, and consent management—reducing regulatory risk as healthcare data breaches continue to rise.
5. Scalable Growth Without Linear Cost Increases
Digital platforms enable providers to expand services like virtual care and chronic disease management without proportional increases in staff or infrastructure, supporting sustainable growth and broader patient reach.
Together, these benefits make medical app development a strategic investment for operational resilience and competitive advantage—not just a digital upgrade.
Benefits for Patients
Healthcare apps significantly improve how patients access, experience, and manage care. When designed correctly, they empower patients while improving health outcomes and continuity of care. Here are 5 key benefits of mobile healthcare app development for patients.

1. Easier Access to Care and Reduced Waiting Time
Patient-facing apps enable online appointment booking, virtual consultations, and digital triage—reducing travel time and long waiting periods. Telehealth solutions have been shown to significantly improve access to care, especially for elderly patients, rural communities, and individuals with mobility limitations.
2. Better Engagement and Self-Management of Health
Healthcare apps help patients actively manage their health through medication reminders, symptom tracking, health education, and personalized care plans. Studies show that digital engagement tools can improve treatment adherence and patient participation, leading to better long-term health outcomes.
3. Improved Care Continuity and Communication
With secure messaging, shared medical records, and care coordination features, patients can communicate more effectively with healthcare providers. This reduces information gaps, minimizes repeated tests, and ensures smoother transitions between in-person and virtual care.
4. Personalized and Preventive Care Experiences
Modern healthcare apps use data and AI to personalize care recommendations, flag potential risks, and support preventive interventions. This allows patients to receive timely guidance based on their medical history, behavior patterns, and real-time health data—rather than one-size-fits-all care.
5. Greater Transparency, Trust, and Data Control
Healthcare apps give patients clear visibility into their medical records, test results, prescriptions, and consent preferences. With built-in security, audit trails, and privacy controls, patients gain more confidence and trust in how their health data is accessed and used.
These benefits transform patients from passive recipients of care into active participants in their health journey, improving both experience and outcomes.
Must-Have Features for a Modern Healthcare App
Healthcare app development solutions must balance usability, security, and regulatory compliance while supporting real clinical and operational workflows. In 2026, the following features are considered essential.
- Secure Authentication & Role-Based Access: Strong login security, multi-factor authentication, and role-based access control ensure that patients, clinicians, and administrators can only access appropriate data.
- Privacy, Consent & Regulatory Compliance: Built-in support for PDPA, HIPAA, and GDPR is critical. This includes data encryption, audit logs, consent management, and clear data access controls.
- User-Friendly & Accessible UX: Healthcare apps must be easy to use for all age groups. Simple navigation, readable design, multilingual support, and accessibility standards are key to user adoption.
- Scheduling, Care Coordination & Communication: Core features such as appointment booking, reminders, secure messaging, and telehealth enable smoother care delivery and better patient–provider interaction.
- System Integration & Interoperability: Seamless integration with EHR/EMR systems, labs, pharmacies, insurers, and medical devices prevents data silos and workflow disruption.
- Analytics, Scalability & Reliability: Healthcare apps should support performance monitoring, reporting, and scalable infrastructure to ensure long-term stability and growth.
These features create a secure, compliant, and scalable healthcare app that delivers value to both providers and patients without unnecessary complexity.
Most Common Healthcare App Use Cases
Healthcare apps are built to solve specific clinical, operational, and patient-experience challenges. Below are the most common healthcare app use cases in 2026, adopted by hospitals, clinics, insurers, and digital health providers.
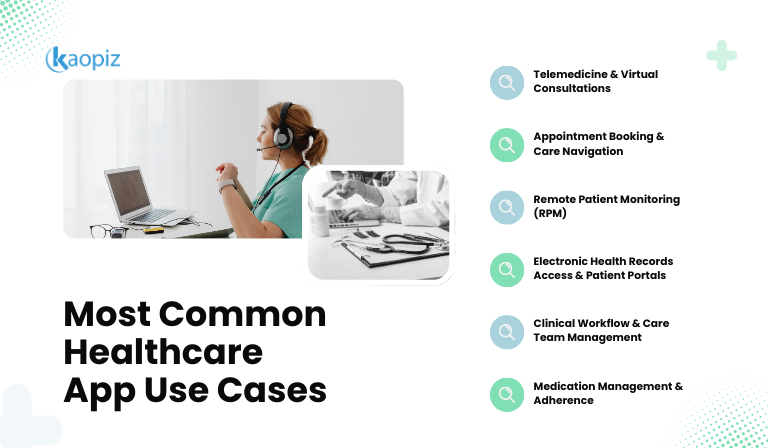
- Telemedicine & Virtual Consultations: Enable remote consultations through secure video, chat, and file sharing. This use case improves access to care, reduces travel and wait times, and supports follow-up visits, chronic care, and mental health services.
- Appointment Booking & Care Navigation: Digital scheduling, reminders, and care navigation tools help patients find the right provider at the right time while reducing no-shows and administrative workload for healthcare staff.
- Remote Patient Monitoring (RPM): Healthcare apps connect with wearables and medical devices to track vital signs, symptoms, and recovery progress in real time. RPM is widely used for chronic disease management, post-discharge monitoring, and elderly care.
- Electronic Health Records (EHR) Access & Patient Portals: Patient portals allow individuals to view medical records, test results, prescriptions, and visit summaries, improving transparency, engagement, and continuity of care.
- Clinical Workflow & Care Team Management: Provider-facing apps support task management, referrals, documentation, and internal communication—helping care teams collaborate more efficiently and reduce errors.
- Medication Management & Adherence: Apps help patients manage prescriptions through reminders, refill alerts, dosage tracking, and drug interaction warnings, improving adherence and treatment outcomes.
The 6 use cases form the foundation of modern digital healthcare ecosystems, often combined within a single platform to support patients, providers, and operations end-to-end.
The 7-Step Simplified Healthcare App Development Process
Building a healthcare app does not need to be complex or high-risk when approached with the right structure. The 7-step simplified healthcare app development process below focuses on clarity, compliance, and measurable outcomes—helping organizations move from idea to deployment with confidence.
Step 1 – Define Scope & Success Metrics
The success of a healthcare app is decided before development starts. Clear scope and success metrics help avoid overbuilding, compliance risks, and costly rework.
First, define core user groups—such as patients, clinicians, administrators, or external partners. Each group has different needs, access levels, and workflows that directly influence features and UX design.
Next, clarify the compliance scope (e.g., PDPA, HIPAA, GDPR) and the types of data the app will handle. Compliance requirements should shape architecture decisions from day one, not be added later.
Finally, identify key integrations (EHR/EMR, labs, insurers, payment systems, devices) and define success metrics such as adoption rate, time saved per clinician, reduced no-shows, or operational cost savings.
Step 2 – Market & Competitor Insights
Before building new features, healthcare organizations should understand what already exists in the market. Market and competitor analysis helps teams avoid reinventing the wheel and making costly assumptions about user needs.

This step involves reviewing similar healthcare apps—both direct competitors and adjacent solutions—to identify common features, UX patterns, pricing models, and compliance approaches. Many core capabilities, such as appointment booking, telehealth flows, or patient portals, already follow proven standards that users expect.
Equally important is identifying gaps and differentiation opportunities. By analyzing user feedback, adoption challenges, and workflow pain points in existing products, organizations can focus development on areas that truly add value rather than duplicating functionality.
Market insights also support better MVP scoping. Instead of building everything at once, teams can prioritize features that matter most, reduce development risk, and launch faster with a validated solution.
Step 3 – UX/UI for Healthcare
In healthcare, user experience directly impacts adoption, safety, and outcomes. A well-designed healthcare app must be intuitive not only for tech-savvy users, but also for elderly patients, caregivers, and busy clinicians.
Healthcare UX should prioritize simplicity, clarity, and accessibility. This includes large readable fonts, high-contrast colors, clear call-to-action buttons, minimal steps per task, and consistent navigation. Complex interfaces increase cognitive load and can lead to errors or user drop-off—especially among older adults.
Accessibility is equally critical. Modern healthcare apps should follow WCAG standards, support screen readers, provide multilingual options, and accommodate users with visual, motor, or cognitive impairments. These considerations are not only best practices but are increasingly tied to regulatory and ethical expectations.
For provider-facing apps, UX should reduce friction in daily workflows. Fast load times, logical information hierarchy, and minimal data entry help clinicians work efficiently without disrupting patient care.
Step 4 – Architecture & Tech Stack Selection
Choosing the right healthcare technology stack is critical to building a secure, scalable, and compliant app. Poor decision at this stage can limit performance, increase long-term costs, and create compliance risks that are difficult to fix later.

Healthcare apps typically require a modular, API-first architecture that supports multiple user roles, system integrations, and future expansion. This often includes a mobile or web frontend, a secure backend, and cloud infrastructure designed for high availability and data protection.
Key mobile healthcare app development considerations when selecting the tech stack include:
- Frontend: Native or cross-platform mobile frameworks and responsive web technologies for performance and accessibility
- Backend: Scalable services that support clinical workflows, data processing, and integration with EHR/EMR systems
- Cloud & Infrastructure: Secure, compliant cloud platforms with backup, monitoring, and disaster recovery
- AI & Data Modules: Optional components for analytics, automation, or decision support
- Security & Compliance: Encryption, access control, audit logging, and compliance-aligned system design
The goal is not to use the newest technologies, but to select proven, healthcare-ready tools that balance performance, maintainability, and regulatory requirements.
Step 5 – MVP Development & Iterations
MVP development allows healthcare organizations to reduce risk and validate value early before committing to full-scale implementation. Instead of building a complete system upfront, teams focus on delivering a minimum set of features that address the most critical user needs.
A healthcare MVP typically includes core workflows, essential compliance requirements, and key integrations—enough to test real-world usage without unnecessary complexity. This approach helps identify usability issues, workflow gaps, and adoption challenges early.
Once the MVP is released, continuous iteration becomes essential. Feedback from patients, clinicians, and administrators is used to refine UX, optimize workflows, and prioritize new features based on actual impact rather than assumptions.
By adopting an MVP-driven approach, healthcare organizations can launch faster, measure results, and evolve their app in a controlled, data-informed way—maximizing ROI while minimizing development risk.
Step 6 – Testing (Security, Compliance, Performance)
Testing is a critical step in healthcare app development, where quality, safety, and trust are validated before real users and sensitive data are involved. Unlike other industries, healthcare apps must meet strict standards for security, compliance, and reliability.

Security testing ensures that patient data is protected through vulnerability assessments, penetration testing, encryption validation, and access control checks. Given the high risk of data breaches in healthcare, security must be tested continuously—not only before launch.
Compliance testing verifies that the app meets regulatory requirements such as PDPA, HIPAA, and GDPR. This includes validating consent flows, audit logs, data access policies, and data retention rules to ensure the system is audit-ready.
Performance and reliability testing confirm that the app remains stable under real-world conditions. Load testing, stress testing, and failover checks help ensure consistent performance during peak usage, system updates, or unexpected traffic spikes.
Step 7 – Deployment, Training & Continuous Improvement
Successful healthcare app development does not end at launch. Deployment must be carefully planned to ensure a smooth rollout with minimal disruption to clinical operations.
This step includes production deployment, data migration (if applicable), system monitoring, and validation in real-world environments. Clear rollout plans—such as phased launches or pilot programs—help reduce risk and allow teams to address issues early.
Training is equally important. Clinicians, staff, and administrators need structured onboarding, documentation, and ongoing support to adopt the system confidently. Well-trained users drive higher adoption and better outcomes.
After deployment, continuous improvement ensures the app remains effective and compliant. Ongoing monitoring, user feedback, performance reviews, and regular security updates allow healthcare organizations to refine features, adapt to regulatory changes, and scale services over time.
Costs of Healthcare App Development in 2026
Healthcare app development costs in 2026 typically range from $30,000 to over $500,000. Simple apps with basic functionality usually cost $30,000–50,000, mid-complexity apps with features like telemedicine or EHR integration range from $50,000–150,000, while enterprise-grade solutions with AI capabilities and multiple system integrations often exceed $150,000.

Final costs depend on feature scope, compliance requirements, development expertise, and whether native or cross-platform technologies are used.
5 Factors Determining Development Costs
- Scope & Feature Depth: The number of features, workflows, and user roles directly impacts development effort. A narrowly scoped MVP costs significantly less than a full-featured healthcare platform built from the start.
- System Integrations: Integrations with EHR/EMR systems, labs, pharmacies, insurers, payment gateways, or medical devices add complexity, testing effort, and long-term maintenance costs.
- Compliance & Security Requirements: Meeting regulations such as PDPA, HIPAA, and GDPR requires built-in security, audit logs, consent management, and rigorous testing—adding necessary but unavoidable cost.
- AI Capabilities (Optional): AI healthcare app development features like symptom checkers, analytics, or decision support increase cost due to data engineering, model integration, validation, and ongoing monitoring.
- Multi-Platform vs. Single-Platform Development: Building for one platform (web or mobile) is more cost-efficient, while supporting iOS, Android, and web increases design, development, and testing effort.
Estimated Timeline and Budget Ranges for a Healthcare MVP
While exact figures vary by region and vendor, typical ranges in 2026 are:
- Basic Healthcare MVP:
- Timeline: 3–4 months
- Budget: $30,000–50,000
- Core features, single platform, limited integrations, baseline compliance
- Mid-Level Healthcare MVP
- Timeline: 4–6 months
- Budget: $50,000–150,000
- Telemedicine or EHR integration, multiple user roles, stronger security
- Advanced MVP / Pilot Platform
- Timeline: 6–8 months
- Budget: $150,000+
- Multi-platform support, AI features, complex integrations, enterprise-grade compliance
Tips: Partnering with an experienced healthcare app development provider—especially through an offshore or hybrid delivery model—can reduce development costs by 40–60% compared to fully in-house or onshore teams. Cost savings come from lower engineering rates, efficient team scaling, and established development processes, without compromising quality or compliance.
Strategic Analysis: Challenges, Decisions, and Investment Readiness
Healthcare app development is not only a technical decision—it is a strategic investment that depends on organizational readiness, market context, and long-term goals. This section helps decision-makers evaluate who should build, what challenges to expect, and when investment makes sense.
Who Should Build a Healthcare App?
Healthcare apps create the most value for organizations that need to scale services, improve efficiency, or deliver digital-first care experiences.
- Clinics & Hospitals: To improve patient access, reduce administrative burden, enable telemedicine, and modernize care delivery.
- Health Centers & Specialty Practices: To streamline scheduling, care coordination, and chronic disease management with focused, workflow-driven solutions.
- Wellness & Healthtech Startups: To launch digital-first products such as fitness, mental health, preventive care, or AI-powered health platforms.
- Insurance Providers: To enhance member engagement, claims processing, preventive care programs, and data-driven risk management.
- Remote Care & Home Healthcare Services: To support virtual consultations, remote patient monitoring, and ongoing care for elderly or chronic patients.
- Corporate Wellness Programs: To deliver employee health platforms focused on prevention, engagement, and population health outcomes.
Challenges in Healthcare App Development & How to Overcome Them
Healthcare mobile application development comes with unique challenges that go beyond technology. The most common risks involve regulatory compliance, system integration, user adoption, and data security. Addressing these challenges early—through the right architecture, UX design, and security practices—significantly reduces project risk and improves long-term success.
| Challenge | Why It Matters | How to Overcome It |
|---|---|---|
| Regulatory Complexity | Healthcare regulations vary by region and impose strict requirements on data handling and auditing | Define compliance scope early and embed security, consent, and audit requirements into system architecture |
| System Integration & Data Silos | Legacy systems and fragmented platforms limit data flow and operational efficiency | Use an API-first approach and prioritize standard healthcare integration protocols |
| User Adoption & Workflow Resistance | Poor UX leads to low adoption among patients and clinicians, reducing ROI | Invest in accessibility, elderly-friendly design, and continuous user feedback |
| Data Security & Privacy Risks | Healthcare data is highly sensitive and a frequent target for cyberattacks | Implement encryption, role-based access control, continuous security testing, and monitoring |
Go/No-Go Analysis: When is the Right Time for Investment?
Not every organization is ready to invest in healthcare app development at the same time. A clear go/no-go assessment helps reduce risk by aligning digital investment with operational readiness, data maturity, and regulatory awareness. The table below provides practical guidance for different types of healthcare organizations.
| Organization Type | Go Signals (Ready to Invest) | No-Go Signals (High Risk) | Recommended Approach |
|---|---|---|---|
| Hospital Groups | Clear operational pain points, leadership buy-in, defined compliance scope | Unclear ownership, limited change management capacity | Start with a focused MVP or pilot before scaling enterprise-wide |
| Insurance Firms | Strong data foundation, digital engagement goals, preventive care initiatives | Legacy-only systems with no integration roadmap | Begin with member portals or analytics-driven digital tools |
| Startups & Digital Health Ventures | Validated problem, early traction, regulatory awareness | Unclear compliance strategy or overreliance on unproven AI | Launch a lean, compliant MVP to test product–market fit |
How to Choose the Right Healthcare App Development Partner
Choosing the right healthcare app development partner is one of the most critical decisions in a digital health initiative. The right partner helps reduce risk, ensure compliance, and deliver a solution that aligns with real clinical and business needs—not just technical requirements.
- Healthcare Domain & Regulatory Expertise: Your partner should demonstrate proven experience in healthcare projects and a clear understanding of regulations. Compliance should be embedded into their development process, not treated as an afterthought.
- Experience with Healthcare Integrations: A strong partner must be comfortable integrating with EHR/EMR systems, labs, insurers, payment platforms, and medical devices. Integration expertise is essential to avoid data silos and workflow disruption.
- Security-First Development Approach: Healthcare apps require advanced security practices, including encryption, role-based access control, audit logging, and regular security testing. Ask how security and compliance are validated throughout the development lifecycle.
- User-Centric & Accessibility-Focused Design: Look for a partner that prioritizes usability, accessibility, and elderly-friendly design. Strong UX capabilities are critical to adoption by both patients and clinicians.
- MVP-Driven & Scalable Delivery Model: The right partner should encourage a phased, MVP-first approach, helping you validate assumptions early and scale only when value is proven.
- Transparent Communication & Long-Term Support: Healthcare apps require ongoing updates, compliance reviews, and performance optimization. Choose a partner that offers clear communication, documentation, and long-term maintenance—not just initial development.
Ultimately, the best healthcare app development partner acts as a strategic advisor, helping you make informed decisions, avoid costly mistakes, and build a solution that delivers sustainable healthcare outcomes.
Why Choose Kaopiz for Healthcare App Development in Singapore
Choosing the right development partner can make the difference between a good healthcare app and a great one. With deep expertise in Healthtech, a proven track record in Singapore’s regulated market, and a commitment to secure, user-focused solutions, Kaopiz is uniquely positioned to bring your healthcare app vision to life.
Why Kaopiz
Kaopiz is a trusted IT outsourcing and software development partner with a team of 700+ professionals having extensive experience in building secure, scalable, and user-friendly healthcare applications. We combine technical excellence, domain expertise, and a compliance-first approach to help clients in Singapore and globally deliver impactful custom healthcare app development services.

What sets us apart:
- Proven healthcare portfolio – Successful projects in telemedicine, patient management systems, and AI-powered health analytics.
- Regulatory knowledge – Familiarity with Singapore’s PDPA and Ministry of Health guidelines, as well as global standards like HIPAA and GDPR.
- End-to-end capabilities – From requirements analysis and UI/UX design to development, integration, testing, and ongoing maintenance.
- Security-first development – Implementation of robust encryption, secure authentication, and regular security audits.
- User-focused design – Multi-language support, intuitive navigation, and accessibility for users across all age groups, including the elderly.
- Agile delivery – Transparent communication, iterative development, and flexibility to adapt to evolving requirements.
By choosing Kaopiz, you gain a long-term partner committed to delivering measurable results, accelerating time-to-market, and ensuring your healthcare app remains competitive in Singapore’s fast-evolving Healthtech ecosystem.
Our Case Studies
Our proven track record in healthcare app development is best demonstrated through real-world projects we’ve delivered for clients. These case studies showcase how Kaopiz transforms ideas into secure, scalable, and user-centric digital health solutions tailored to Singapore’s market needs.
Muscle Health Management
QuantumTX develops medical and fitness devices using Magnetic Muscle Energetic Training and its proprietary Magnetic-Mitohormesis technology to deliver exercise benefits without physical strain.

Challenges: Manual workflows caused inefficiencies, errors, and limited scalability. Reliance on third-party systems reduced flexibility and control.
Kaopiz Solutions: Kaopiz built a web and mobile app to streamline client management, scheduling, payments, assessments, and progress tracking. Administrators gained tools for partner center oversight, business insights, and promotions, while users could book appointments, track progress, and access resources anytime.
Results:
- Higher efficiency through automation of operations.
- Lower costs by reducing reliance on third-party tools.
- Better decisions via centralized dashboards and analytics.
“We highly appreciate the technical expertise, dedication, and consistent delivery quality that Kaopiz has demonstrated over the years. Their team has been a reliable and capable technology partner for our projects.” — Kai Zhien Chan, Product Manager, QuantumTX.
AI-Powered Fitness App
A fitness and wellness company aiming to enhance workout effectiveness and user engagement through advanced technology.
Challenges: The client needed a solution to ensure users maintain proper exercise form, boost motivation with interactive features, and simplify progress tracking and in-app purchase management.
Kaopiz Solutions: We developed an AI-driven mobile app that uses camera-based motion analysis to assess user movements, providing instant feedback and performance scores. Gamified features like quests, rankings, and virtual pets increase engagement, while an admin dashboard enables efficient management of users, content, notifications, and sales.
Results:
- Improved workout quality through real-time form correction.
- Higher user engagement with gamification and rewards.
- Simplified management for business growth via a centralized admin dashboard.
Hypertension Management App
A healthcare organization specializing in chronic disease management wanted a mobile app to improve treatment outcomes for hypertensive patients by making at-home blood pressure tracking easier and more engaging.
Challenges: Traditional tracking methods were tedious, leading to poor patient adherence. The client needed a tool that simplified measurements, visualized trends, and motivated daily use.
Kaopiz Solutions: We built a mobile app that connects directly with blood pressure monitors, provides real-time readings, and sends visual and audio alerts for abnormal values. To increase engagement, we introduced a gamified aquarium-themed interface that rewards consistent monitoring.
Results:
- Better adherence to treatment plans through interactive design.
- Higher measurement accuracy with guided monitoring.
- Fast delivery — completed in 2 months, fully compliant with healthcare standards.
Emerging Trends Transforming Healthcare Apps in 2026
Healthcare apps in 2026 are shifting from basic digital tools to intelligent, connected, and patient-centric platforms.

Several key healthcare app trends are driving this transformation.
- AI-Driven Insights & Automation: AI is increasingly used for clinical decision support, workflow automation, and data analysis—helping providers improve efficiency and care quality when applied responsibly.
- Virtual-First & Remote Care Models: Telemedicine, remote monitoring, and hybrid care models are becoming standard, enabling continuous care beyond physical facilities.
- Interoperability & System Connectivity: API-first architectures and data standards allow healthcare apps to integrate seamlessly with EHRs, labs, insurers, and partner systems, reducing data silos.
- Accessibility & Patient-Centric Design: Elderly-friendly UX, accessibility standards, and multilingual support are now essential for adoption and inclusive care.
- Privacy-First & Cloud-Native Platforms: Healthcare apps prioritize security, consent management, and cloud-native scalability to meet regulatory demands and support long-term growth.
Together, these trends are shaping safer, smarter, and more scalable healthcare apps in 2026.
Conclusion
Healthcare app development in 2026 is no longer just a technology initiative—it is a strategic decision that directly impacts care quality, operational efficiency, and long-term sustainability. Successful healthcare apps are built on clear scope definition, strong compliance foundations, user-centric design, and a phased, risk-reduced development approach.
By understanding use cases, costs, challenges, and investment readiness, healthcare organizations can make informed go/no-go decisions and avoid costly missteps. Starting with a focused MVP, validating real-world impact, and scaling based on proven value remains the most effective path forward.
FAQs
- How Much Does It Cost to Develop a Healthcare App in Singapore?
-
Healthcare mobile app development costs vary based on features, complexity, platforms (iOS, Android, or both), and integrations such as EHR systems or wearable devices.
On average, a basic healthcare app starts from SGD 40,000, while advanced, fully integrated solutions can exceed SGD 500,000. - How Do I Ensure My Healthcare App Meets Singapore’s Regulations?
-
You must comply with the PDPA, relevant Ministry of Health (MOH) guidelines, and security best practices such as encryption and access controls.Partnering with an experienced healthtech developer like Kaopiz ensures compliance is built in from day one. - Can Kaopiz Develop Both Patient-Facing and Provider-Facing Healthcare Apps?
-
Yes. Kaopiz has delivered both patient-facing apps (telemedicine, wellness tracking) and provider-facing systems (EHR access, hospital management), including hybrid platforms that connect both sides. - How Long Does It Take to Develop a Healthcare App in Singapore?
-
Development timelines depend on scope and complexity. A Minimum Viable Product (MVP) typically takes 3–4 months, while feature-rich apps with multiple integrations may require 6–9 months or longer. - What Technologies Are Used in Healthcare App Development?
-
Common technologies include Flutter or React Native for cross-platform apps, Swift for iOS, Kotlin for Android, and Python, Node.js, or Java for backend development. Integrations often involve APIs for EHR systems, payment gateways, AI analytics, and IoT medical devices.
2 Replies to “Healthcare App Development: The 7-Step Simplified Guide [2026]”
Leave a Comment
Trending Post



















Pingback:10 Healthcare Software Development Trends in Singapore 2025
Pingback:Top Healthcare App Development Companies in Singapore (2025)